Focal Sclerosing Osteomyelitis, also referred to as Condensing Osteitis is a condition in which the tissues around the root are infected or it is the periapical inflammatory condition. It is not a commonly encountered situation.
Although its occurrence is rare, it can be seen in individuals who maintain good oral hygiene. Here is some important information to guide you about the basic features, symptoms, diagnosis, and management of the rare condition of the tooth.
What is it?
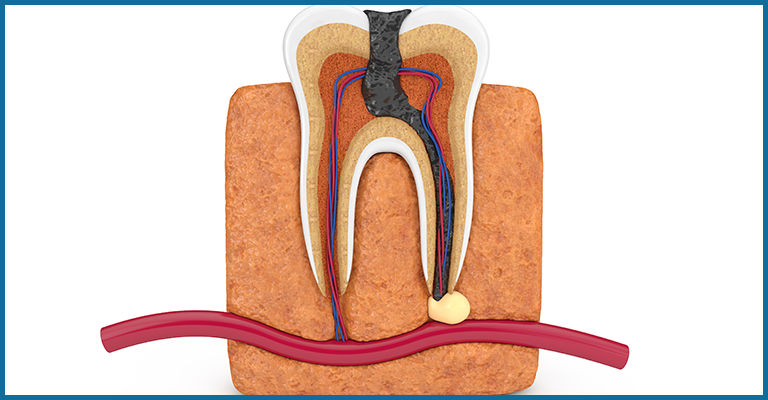
The tooth is composed of two parts: the crown and the root. The portion of teeth visible inside the mouth is the crown while the part embedded inside the jaw bone is known as the root. The region around the apex or the tips of the roots is known as the periapical area. Condensing osteitis is an inflammatory disease of the periapical region. Most of the time it is considered a stimulus to the inflammatory response.
Usually, the response to inflammatory reaction is bone destruction but here, the response is the deposition of bone instead. Therefore, the lesion due to infection here is radiopaque and not radiolucent. A radiopaque lesion is the one when x-rays pass through a dense structure, that is, it prevents the rays to pass.
Symptoms
This condition is usually symptomless with occasional episodes of pain, therefore can be diagnosed through an x-ray by your endodontist.
Condensing osteitis is mostly seen in young adults but can be noticed in other age groups too.
There is a predilection (more common) for this condition in the molar region but can be seen in other teeth regions too.
Diagnosis and Management
Whenever condensing osteitis is suspected, the first and foremost step is the referral to an endodontist. The management is initiated with a thorough examination of the infected tooth.
The endodontist will check the pulp tissue of the tooth for vitality. The pulp tissue is the innermost soft tissue of the tooth that contains nerves and blood vessels and maintains the vitality of the tooth as it provides nutrition.
This can be done through various methods of pulp vitality testing. The choice of the test depends on the primary complaint of the patient.
If there is necrosis or dead tissue in the pulp or if the inflammation is severe then the last resort is to extract the tooth and it cannot be saved.

Prognosis
To add to your surprise, if the bone deposited due to infection is not causing any symptoms and discomfort then there is no need for management and the tooth can be left as such.
It is observed that such tooth remains normal and can function normally for years without any inconvenience.
But remember a periodic examination is necessary where your endodontist can look for changes through x-rays. If required, the treatment can be done. In cases where the affected tooth has been extracted the socket that is left after extraction is the area of condensing osteitis of the jaw, and can be left as such. It is painless and known as osteosclerosis of the bone scar.





